Meldung vom:
Smartwatch Data: Interdisciplinary Team Finds Early Health Differences in Long COVID Patients
About the study
The study “Wearable Data Reveals Distinct Characteristics of Individuals with Persistent Symptoms after a SARS-CoV-2 InfectionExterner Link,” by K. Ledebur, M. Wiedermann, C. Puta, S. Thurner, P. Klimek, and D. Brockmann, was published in npj Digital Medicine (doi: 10.1038/s41746-025-01456-x).
People who later experienced persistent shortness of breath or fatigue after a COVID infection were already taking significantly fewer steps per day and had a higher resting heart rate before contracting the virus, according to a CSH study published in npj Digital MedicineExterner Link. This may indicate lower fitness levels or pre-existing conditions as potential risk factors.
HIGHER RESTING HEART RATE AND 3,000 FEWER STEPS
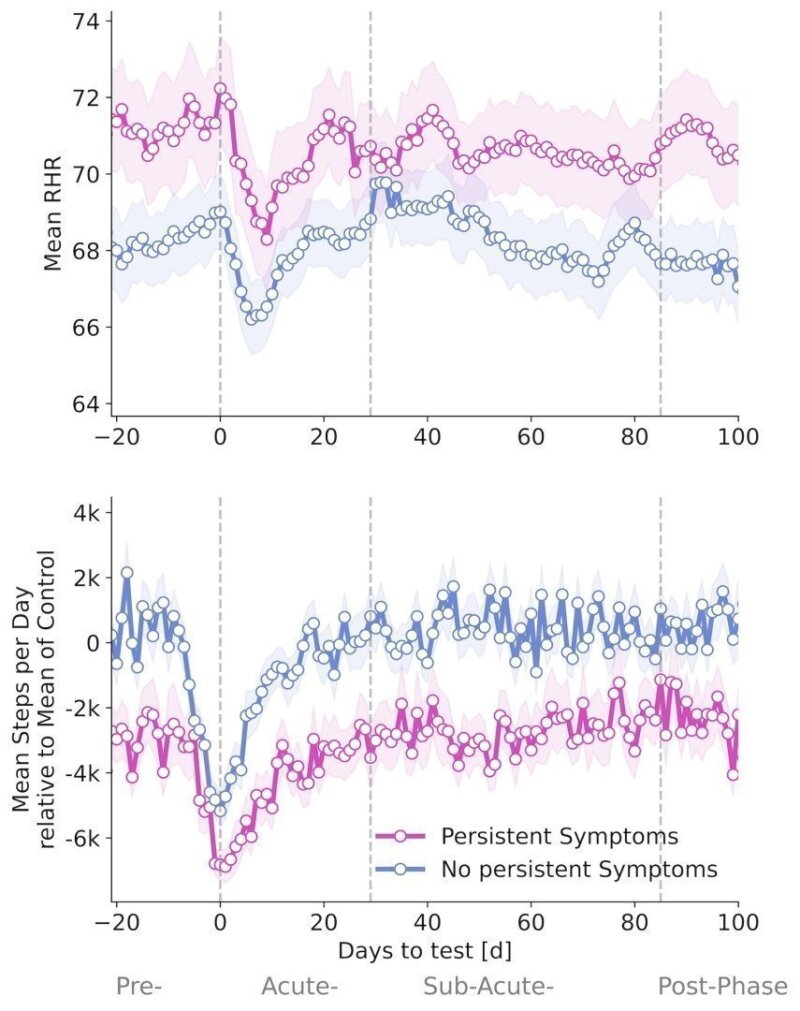
People with persistent symptoms showed significant differences in activity levels and resting heart rate compared to others. “In the three weeks before infection, patients who later reported persistent symptoms took an average of just 5,075 steps per day—about 3,030 fewer than SARS-CoV-2 patients who recovered without persistent symptoms,” says Katharina Ledebur (first author of the study).
RESTING HEART RATE AND INFECTION ASSOCIATED BRADYCARDIA
Resting heart rates also showed differences before infection. Those who later developed persistent symptoms had a resting heart rate 2.37 beats per minute higher than individuals who recovered without lingering effects.
Both groups exhibited a pattern of infection based heart rate changes. Individuals with persistent symptoms (M-COVID-19[+]PS) had a transient tachycardia followed by prolonged relative bradycardia, which did not return to baseline until 18 days after infection. The relative bradycardia of M-COVID-19[+]NS individuals (non-persistent symptoms) persisted until 15 days after infection.
Mean resting heart rate (top) and mean daily steps relative to the average of individuals with COVID infection but without persistent symptoms (bottom) before, during, and after a COVID infection. The pink line represents patients who developed persistent symptoms, while the blue line represents those who did not. © Complexity Science Hub
Grafik: Ledebur
TWO PERSISTENT SYMPTOMS
For the study, researchers divided smartwatch and fitness tracker data into four phases: before infection, during the acute infection (0 to 4 weeks after a positive test), the subacute phase (5 to 12 weeks after a positive test), and the post-acute phase (beyond 12 weeks).
Participants also completed monthly and weekly surveys about COVID-19 tests, their subjective well-being, and ongoing symptoms. “Using these symptom reports, we found that among 11 symptoms analyzed, only shortness of breath and fatigue persisted beyond the acute phase of SARS-CoV-2 infection. Other symptoms, such as cough, headache, or fever, showed no long-term effects,” Ledebur explains. Overall, 2.6% of all SARS-CoV-2-positive individuals reported prolonged shortness of breath, 10.4% experienced long-lasting fatigue, and 1.8% had both symptoms.
Data indicate that long COVID is not a problem of deconditioning alone
The data of the study indicate that long COVID is not a problem of deconditioning alone. Both the persistent symptoms group and the no persistent symptoms group returned to their baseline values after infection.
“What was surprising was that, for both groups, heart rate and step count eventually returned to pre-infection levels,” Ledebur notes. “Despite ongoing shortness of breath and/or fatigue, affected individuals took as many steps as they did before infection,” says Ledebur.”
Complexity Science Hub: